Induction of labour works by mimicking (copying) the natural process of labour. It can be broken down into 3 steps:
- Ripening your cervix
- Breaking your waters
- Starting or boosting your contractions
IMPORTANT TO KNOW:
It may take a few days for labour to start.
Induction is a process with many steps but not everyone will have to go through all of the steps. Your labour may start and/or progress with one, some or all of these interventions.
You may be offered a combination of methods depending on your individual circumstances.
You can pause the process at each step before deciding what to do next. It is always your choice and you can talk about the benefits, risks and alternatives specific to your circumstances (the BRAIN questions) before considering your options, including stopping and waiting for a while.
NICE (National Institute for Health & Care Excellence) publishes national guidelines for clinical care. To access the guidelines on induction of labour, visit the NICE website at www.nice.org.uk.
Step 1: Ripening your cervix
Membrane Sweeps
Membrane sweeps involve having a vaginal examination where the midwife or doctor places a finger inside your cervix and makes a circular ‘sweeping’ movement to separate the membranes from the cervix. This increases the production of a hormone called prostaglandin which can encourage labour to start. Some evidence suggests membrane sweeps increase the chances of labour starting naturally (Cochrane review, 2020).
Membrane sweeps can be offered to you by your community midwife and can be performed in a clinic. These would usually be offered when you’re around 40 weeks pregnant. Sweeps may also be offered earlier than 40 weeks by your consultant obstetrician if they think that this would benefit you.
A sweep is an internal examination and may be uncomfortable. Your midwife will talk you through what they are doing, and you can ask them to stop at any time.
The sweep can stretch your cervix, and you may experience a minimal amount of bleeding (spotting) afterwards. You may also have a “show” later in the day. A “show” is a plug of mucus, sometimes brown or spotted with blood, which is released as the cervix begins to open. This is normal and will not cause harm to your baby.
A sweep should not cause heavy bleeding, and you should contact the hospital urgently if this occurs.
Cervical Ripening Balloon (CRB)
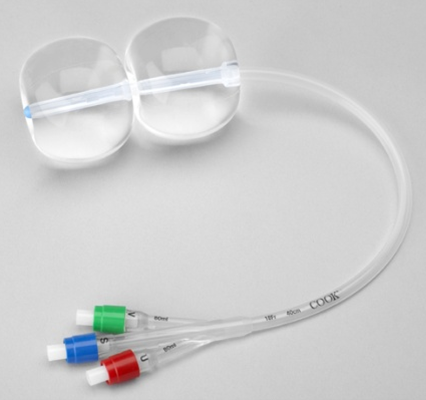
A cervical ripening balloon (CRB) is a silicone tube which has two inflatable balloons. The balloons are inflated with sterile water. This is a safe, drug-free, mechanical method of ripening the cervix. At present, you would need to attend the hospital to have a CRB inserted.
The CRB is inserted either during a vaginal examination or with a speculum (this is a device used by medical professionals to assist a vaginal examination). The top balloon is inflated in your uterus (below baby’s head) and the bottom balloon is inflated below your cervix (at the top of your vagina), as pictured. The tube will hang down outside your vagina. It can be easily folded to sit between two pairs of underwear for your comfort.

The constant, gentle pressure applied to both the inside and outside of your cervix increases the natural production of the hormone prostaglandin, similar to a membrane sweep. This helps the cervix to ripen and dilate, although it may not cause contractions to start. After insertion you may experience some mild to moderate cramps (like during a period), usually for 2-3 hours, but these usually wear off.
The CRB stays in place for a minimum of 12 hours and a maximum of 24 hours and is removed by deflating the balloons. Once removed you will be offered a vaginal examination to assess if your cervix is dilated enough to have your waters broken.
Advantages
- A 2019 Cochrane review concluded that a CRB is as effective as synthetic prostaglandins (medications) at ripening the cervix, and that there is little difference in the length of labour and the chance of needing a caesarean birth (Mechanical methods for induction of labour | Cochrane).
- The same review concluded that a CRB may be safer for your baby as it reduces the chance of uterine hyperstimulation (too strong or too long contractions).
Disadvantages
- CRBs are mechanical methods of ripening your cervix. They may not cause contractions to start, which may mean you will need medications to help your labour establish.
- There is a theoretical slight increase in the chance of you or your baby developing an infection with a CRB. This is because part of it is inserted into the uterus. However, the CRB itself is sterilised (clean) within its packaging, and the insertion technique we use minimises the chances of any contamination.
- You may experience some discomfort as the CRB is inserted as the cervix has to be manipulated slightly to allow the tubing through.
- If your cervix is completely closed or in a very posterior position it may not be possible to insert a CRB. In this situation, synthetic prostaglandins (medications) will be recommended.
- If during a vaginal examination the midwife or doctor finds that your baby’s head is too high up in your pelvis then a CRB should not be used. In this situation, synthetic prostaglandins will be recommended.
- Sometimes the CRB is not effective at ripening your cervix enough to allow your waters to be broken after 24 hours. In this situation, synthetic prostaglandins may be recommended to help ripen your cervix.
Synthetic Vaginal Prostaglandins
Synthetic vaginal prostaglandins are an artificial hormone which mimic (copy) the action of the natural prostaglandins which your body produces. This helps to ripen your cervix.
There are two methods used to deliver the artificial hormone:

- The first method we use is called Propess. This is a pessary within a small, flat tampon that is placed behind your cervix during a vaginal examination. A small amount of the tape will hang out of the vagina for easy removal of the pessary. The pessary will stay in for a maximum of 24 hours and once removed you will be offered a vaginal examination to assess if your cervix is dilated enough to have your waters broken.
- The second method we use is called Dinoprostone. It comes in tablet form and is similarly placed behind your cervix during a vaginal examination. This method is used when the Propess pessary has not been effective enough in dilating your cervix. The tablet will melt over 6 hours at which point we will offer do an examination to check if it has been effective. You may have up to two rounds of the Dinoprostone tablet.
Advantages
- This method may be sufficient to start your labour which will then progress naturally.
Disadvantages
- You may experience some discomfort as the synthetic prostaglandins are inserted. We use plenty of lubricating gel to prevent this, but the pessary or tablet may feel a bit uncomfortable to begin with.
- Sometimes synthetic prostaglandin can cause you to have too many contractions (more than five in a 10-minute period). This is known as uterine hyperstimulation and can affect your baby’s heartrate and oxygen levels. You will be monitored closely and this can be controlled if it happens.
Step 2: Breaking your waters
Once your cervix has softened and ripened it is usually a few centimetres dilated. The next stage of the induction of labour process is to encourage your waters to break. This allows your baby’s head to descend further into your pelvis and put pressure on your cervix. This pressure helps to stretch the cervix, and stretch receptors contained within the muscle of the uterus and cervix send messages to the pituitary gland to encourage oxytocin release. This oxytocin release causes contractions to start which in turn push your baby further down into your pelvis, increasing pressure on the cervix and causing it to dilate. This continual feedback loop is known as the Ferguson reflex; it helps to establish and progress your labour.
Spontaneous Rupture of Membranes (SRM)
Your waters may break by themselves (spontaneously) during the induction process. Sometimes this may happen as a large gush of fluid, or you may notice a continuous slight trickle of watery discharge from your vagina. If you think your waters have broken, please inform a midwife immediately.
Artificial Rupture of Membranes (ARM)
This is the process of “breaking your waters” and can be offered if the cervix has started to ripen and is around 2cm dilated. If you agree to have your waters broken at this stage, a vaginal examination is performed by the midwife or doctor, who will insert two fingers through your cervix and use a slim, sterile, plastic instrument to make a hole in the membranes that contain the amniotic fluid around your baby. This can only be performed on the labour ward, not on the antenatal ward or in the birth centre.
For some women this is enough to stimulate labour and contractions naturally, and you can choose to wait and mobilise for up to 4 hours to see if this happens. If you have not had a baby before, it is recommended you begin the drip immediately after you have an artificial rupture of membranes because it is unlikely your contractions will start spontaneously.
What if your cervix hasn’t ripened enough for your waters to be broken?
If the Cervical Ripening Balloon (CRB) or vaginal prostaglandins have not been fully effective at ripening your cervix, you will have the opportunity to discuss your options with the midwives and doctors. This discussion will take into account your personal circumstances and preferences, and a plan will be made with you to pause or continue your induction, or consider a caesarean birth.
Step 3: Starting or boosting contractions with a hormone drip
If you are not having any contractions within 4 hours of your waters being broken, then a hormone drip (intravenous oxytocin) will be recommended. We use a synthetic form of oxytocin (Syntocinon) to help start and make your contractions stronger. This hormone is delivered by an intravenous drip (through a small tube which is infused into a vein in your arm or hand). The drip can be adjusted according to how your labour is progressing. The aim is for the uterus to contract regularly until you give birth.
During the time you are on the hormone drip, we recommend monitoring your baby’s heartbeat continuously using a cardiotocograph (CTG). This is to make sure we can pick up any changes to your baby’s heart rate which may be a sign they’re in distress. Your ability to walk around may be limited by the drip and the CTG, but your midwife will be able to support you into active birth positions that are comfortable for you, whether it is standing or using a birthing ball. It is not advised that you use a bath or pool whilst having intravenous oxytocin due to the electrical equipment used.













