After an operation it is normal to expect a degree of discomfort or pain. Pain after surgery is known as acute pain; it has a known cause and will improve as the tissues heal. The amount of pain will reduce quickly in the first few days. In the meantime good pain relief is important.
This webpage gives you information on the pain relief options which may be available to you after surgery. Methods of pain relief are constantly improving, and you will be able to get moving again sooner after your surgery than you might expect.
The Inpatient Pain Management Team, and the staff on the ward, are here to make sure any pain you do have is as well controlled as possible.
If you have any concerns about how your pain will be managed after surgery then please discuss these at your pre-assessment appointment or with your anaesthetist.
If you suffer from chronic pain, or take regular strong pain medication, the Acute Pain Team will be informed before your surgery to plan for any potential problems. You should take your usual pain medicines on the morning of surgery unless you have been told not to by a doctor or nurse.
Aims of pain relief
It will not be possible to remove all pain, but we would expect you to be comfortable enough to make progress with your recovery.
Getting moving and returning to normal activities are crucial to helping you recover faster, return to a good quality of health and avoid complications. Pain relief is designed to make this possible.
The aims of pain relief after surgery are to:
Allow you to get moving
- Helps to prevent muscle weakness, stiffness, constipation and blood clots
Allow you to deep breath and cough
- Helps prevent chest infections or pneumonia
Allow you to return to your normal activities
- While your body continues to heal
Improve sleep
- Important for physical healing and mental wellbeing
Improve mood and anxiety
- Important for all aspects of your recovery
Getting the balance right
Pain relief is important to help you recover. However, pain medicine may have side effects. It is important to get the balance right and we are here to help you do this.
What does good pain relief feel like?
TOO MUCH
Comfortable but problems with side effects from pain killers. These might be feeling sick, itch, constipation or feeling very tired.
Speak to the nurses and doctors looking after you. They will give you advice or make changes to your pain relief.
JUST RIGHT
Mild pain but comfortable. You should be able to move, deep breathe, and cough while keeping a smile on your face!
Keep going as you are and aim to gradually reduce the amount of pain relief you are using.
NOT ENOUGH
Severe pain on movement, only able to take small breaths and not able to cough.
You don’t need to struggle on. Tell the nurses or doctors looking after you that you are in pain and they will help.
Speak to the nurses and doctors looking after you. They will give you advice or make changes to your pain relief.
Keep going as you are and aim to gradually reduce the amount of pain relief you are using.
You don’t need to struggle on. Tell the nurses or doctors looking after you that you are in pain and they will help.
Managing pain after surgery is a team effort, involving you and the staff looking after you. If at any point you feel your pain control could be better, you should discuss this with the doctors and nurses on the ward or the Inpatient Pain Management Team.
The acute pain team
If you have a major operation, the Inpatient Pain Management Team may be involved in your care and will visit you on the ward if required.
The Inpatient Pain Management Team work closely with you, and the doctors and nurses on the ward, to make sure your pain is as well controlled as possible.
Who are the acute pain team?
SPECIALIST NURSES
Very experienced in managing acute pain after surgery.
PAIN CONSULTANT
Specialist in pain medicine.


ANAESTHETIST
Specialist training in pain medicine. They are on call 24 hours a day.
What do the pain management team do?
During each visit the Inpatient Pain Management Team will:
Assess your pain
You will be asked to describe your pain, including whether it is mild, moderate or severe. You may also be asked to give your pain a score out of 10, where 10 is the worst pain and 0 is no pain.
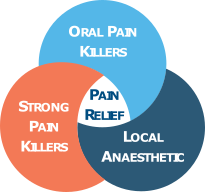
A combination of methods is good because each one works on a different part of the pain system. Also, it stops you needing large doses of any single medicine, so the risk of side effects is reduced.
Oral painkillers
You will be given regular painkillers as either tablets or liquid. Examples include paracetamol, ibuprofen and tramadol. Although they may seem simple, they are very important. Each one works in a different way and they are the building blocks on which any pain management plan is built.
Strong painkillers
You are likely to require other strong painkillers. These are medicines such as morphine, fentanyl or oxycodone. They are all types of painkillers called opioids. Opioids are good at controlling acute pain after surgery.
They can be given to you in different ways:
Short acting
Tablets or liquid which you take when your pain gets worse or before you are going to move about.
Patches
These stick to your skin and provide background pain relief throughout the day and night.
Long acting
Tablets which you take twice a day and provide background pain relief for 12 hours.
Patient controlled analgesia (PCA)
A PCA is a machine connected to your drip, with a button for you to press. Each time you press the button you receive a small dose of painkiller through the drip. The machine controls how often you can get a dose to stop you accidentally taking too much.
Are opioids safe?
You may have heard stories about problems with opioids, especially people becoming addicted. When used for a short time to help with acute pain after surgery the risk of becoming addicted is very small.
The Inpatient Pain Management Team will always make sure there is a plan in place to reduce the amount of opioids you are taking as your pain improves. Opioids do not work for long-term, or chronic pain.
Local anaesthetic
For surgery on your abdomen or legs, a regional anaesthetic may be used. This is usually a spinal or an epidural.
These are injections in the middle of your back which are performed when you are awake, before you are given a general anaesthetic to make you unconscious for the operation.
EPIDURAL
A very small plastic tube, known as a catheter, is inserted through a needle.
Local anaesthetic and painkillers can be given through the tube for up to 3 days after the operation.
SPINAL
You are given a single injection in your lower back of local anaesthetic and strong painkiller.
This provides good pain relief for up to 24 hours after surgery.
- The injections are usually done with you sitting up, although they can also be done with you lying on your side.
- Local anaesthetic is injected to numb the skin before the spinal or epidural injection starts.
- More local anaesthetic drug, and a strong painkiller, is injected through a needle close to the nerves in your back which detect pain from your abdomen.
Regional anaesthetic provides good pain relief after surgery and reduces the amount of strong painkillers you need to take. This helps you get moving sooner and reduces the risk of side effects from painkillers.
The options available will be discussed with you by your anaesthetist, who will also explain any risks of these injections.
Feeling sick
Some patients can feel, or be, sick after an operation. This can be because of the anaesthetic, the surgery or the painkillers you are taking.
Anti-sickness medicine will always be available to you. So if you are feeling sick, please let a member of staff known so that it can be treated.
Relaxation and distraction
Hospitals can be a busy and stressful environment. You may find it useful to bring something to help you relax. For example, this could be something to read, or some music to listen to.
Going home
As you recover from your operation your pain will improve. The amount of pain medicine you need will decrease.
By the time you are ready to go home, you may still be taking some painkillers. It is important that you continue to gradually reduce the amount you are taking after you go home. The Inpatient Pain Management Team will help provide you with a plan for how to do this.
If you are taking long-acting opioids, you should aim to gradually reduce and stop these within 2 weeks. You may need the occasional dose of short-acting opioid, but should not be using these for longer than 4 weeks after you go home.
If you feel like you still need strong painkillers for more than 4 weeks after going home, it is important to discuss this with your GP.
Research
NHS Lothian is committed to supporting clinical research. If you are eligible for any research studies, someone from the research team may contact you with information that you can read. If you do not wish to take part in any research, this will not affect your clinical care in any way.
PLEASE NOTE
This website includes content taken from the Royal College of Anaesthetists’ (RCoA) leaflets ‘Fitter, Better, Sooner (2018)’, ‘You and your anaesthetic (2020)’, ‘Anaesthesia explained (2015)’, and ‘Common events and risks in anaesthesia(2019)’. However, The RCoA has not reviewed the website as a whole. Some of the RCoA infographics used on the website have been adapted for web viewing.














