Going home from hospital after surgery is a really positive step in your recovery. It means you can continue increasing the amount you are moving and start returning to normal activities.
During your time in hospital you will have received excellent support from a whole range of professionals. For some people, going home may be a daunting step. But it is important to know that leaving hospital does not mean you are leaving this support behind.
This webpage provides answers to some of common questions about going home after surgery. There is also information about how to access additional support should you need it.
A helping hand

Recovering from surgery puts a physical strain on your body. It is important to keep moving to improve your recovery and reduce the risk of complications. But it is also likely you will be more tired than normal. Make sure you get plenty of rest as well as staying active.
This is where some extra help from your friends and family can be very important. Preparing to go home after surgery can begin even before you come to hospital. It may be worth making arrangements with friends and family, even before you come to hospital.
This might include getting help with looking after children, elderly relatives or pets, or help with shopping and cooking after you get home.
Eating and drinking
After surgery, you should aim to eat a healthy balanced diet to provide the energy and nutrients your body needs to recover. You should also keep yourself well hydrated.
You may find that your appetite is reduced. It may be easier to eat and drink small amounts more often. You may find foods affect you differently. Introducing foods gradually in small portions can help identify any which cause problems.
Bowel habit
If you have had abdominal surgery, it is not unusual to have a change in your bowel habit. It may take several months for your bowel movements to return to normal, however these changes usually settle with time.
Constipation
- Drink plenty of fluids – aim for 8 – 10 cups per day
- Eat food high in fibre such as wholemeal bread or cereal or fruit and vegetables
- Mobilise early after surgery
Diarrhoea
- Drink plenty of fluids to avoid dehydration
- Reduce high fibre foods for a short period of time
- Avoid fatty or fried foods, spicy food and tea or coffee
- Eat little and often
If you continue to lose weight after your operation, please speak to your GP. They will be able to give you some advice and may refer you to a dietician.
Mobility and exercise
It is important to keep active during your recovery – this has many benefits:
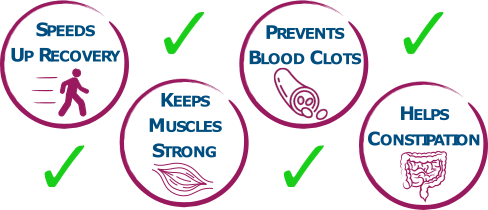
You should gradually increase the amount you are doing each day, aiming to walk a little bit further, or for a bit longer, each time.
Why not ask your family and friends to help you with this? Visits and phone calls from family and friends can cheer you up and encourage you to reach your goals.
Rest to recover
Recovering from surgery puts an extra physical strain on the body. So it is important when you are not being active that you get good amounts of rest.
Good quality sleep is also really important. Be careful that you don’t tire yourself out from too many visitors.
Pain relief
As you recover from your operation your pain will improve. The amount of pain medicine you need will decrease.
By the time you are ready to go home, you may still be taking some painkillers. It is important that you continue to gradually reduce the amount you are taking after you go home. The doctors and nurses will help provide you with a plan for how to do this.
If you are taking strong painkillers, such as long-acting opioids, you should aim to gradually reduce and stop these within 2 weeks. You may need the occasional dose of short-acting opioid, but should not be using these for longer than 4 weeks after you go home.
If you feel like you still need strong painkillers for more than 4 weeks after going home, it is important to discuss this with your GP.
Day surgery
After some operations, it may be possible for you to go home the same day as your surgery. This is called Day Surgery.
If you are going home the same day as your surgery you will not be allowed to drive home. You will need a responsible adult to pick you up, or accompany you in a taxi, and someone to be at home with you for at least 24 hours after the operation.
Remember that if you have had a general anaesthetic, for the first 24 hours make sure you:
- Do not drive or operate any mechanical or electrical machinery
- Do not sign legal documents
- Do not drink alcohol or take sleeping tablets
Wound care
Before you leave hospital the nurses will show you how to look after your wound and provide you with spare bandages and dressings.
If you have stitches, or staples, that need removed you should make an appointment with the nurse at your GP surgery 10 – 14 days after your operation.
It is important that you keep your wound clean and dry to give it the best chance of healing.
You should look out for signs of a wound infection:
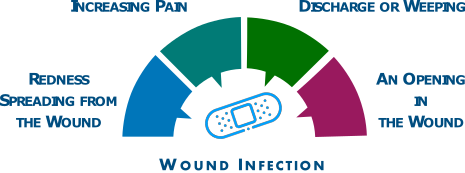
If you have any concerns about your wound, please speak to your GP or call NHS 24 on 111
Driving
If you drive, it is important that you do not return to driving before you are ready.

Strong painkillers can affect your concentration and make you more sleepy. You should not drive while you are still taking strong painkillers.
There are two important tests you should do to check that you are ready to drive:
- Make an emergency stop without pain – sit in the driver’s seat and press very firmly on the brake pedal to check
- Be able to turn freely to look over both shoulders – make sure you can easily see both blind spots
If you have any concerns about your ability to drive you should speak to your GP. If you are still not able to drive 3 months after your operation you should tell the DVLA.

Click here to visit the DVLA website
You could be fined up to £1,000 if you do not tell DVLA about a condition that might affect your ability to drive safely. You could also be prosecuted if you have an accident.
Time off work
If you work, the amount of time you need off will be different for everybody. It will depend on the:
- Type of operation you’ve had
- Type of job you do
- Speed of your recovery
Speak to the doctors looking after you in hospital before you leave about how much time you should take off.
Phased return
Returning to normal activities, including returning to work, is an important part of your recovery.
You should speak to your employer about going back to work. It may be possible for you to have a phased return. This is where you return to work but do fewer hours, or less physical work, at the start, and then gradually increase how much you do.
Letter for your employer
If you need less than 1 week off work you do not need a letter from a doctor and can self-certify.
If you are likely to need more than 1 week off work the doctors on the ward can give you a letter before you leave hospital. If you end up needing longer off work than originally planned, you should speak to your GP.
Getting home
You won’t be able to drive home after your operation and will need a responsible adult to pick you up, or accompany you in a taxi.
Before you leave the hospital the nurses will go through your medication with you. They will tell you about any changes to your mediation or any new medicines. They will also make sure you have a good supply of each medicine.
When you leave hospital, a letter will be sent to your GP telling them about your operation and any changes to your medicines.
Discharge lounge
The discharge lounge is a comfortable and relaxed environment in which you can wait to be collected by friends, family or patient transport.
On the day your are due to go home, you may be moved to the discharge lounge to allow your bed to be available for another patient.
The discharge lounge is located on the ground floor near the rear main entrance.
For more information see the Discharge Lounge: Information for patients leaflet
Caring for someone who has had a general anaesthetic or sedation
The Royal College of Anaesthetists have provided an excellent resource called Caring for someone recovering from a general anaesthetic or sedation
We suggest that you and the person looking after you read this thoroughly.
Sources of support
Once you are home from hospital there are several places you can get support or advice if you need it.
Who can I call?
Depending on what type of surgery you have had, you may be given the details of a patient advice line if you have concerns after your operation.

There are lots of other people who can also help you after your surgery:
GP AND NHS 24
For all other concerns not relating to your operation, please contact either your own GP or NHS 24 by phoning 111.
If you feel it is an emergency, you should dial 999 and inform them about the problem that you are having and that you have had recent surgery
STOMA NURSE
If you have a stoma, a Stoma Nurse will give you information about how to look after your stoma and what diet to eat.
If you have any concerns about your stoma after you leave hospital, you should contact the Stoma Nurses.
SPECIALIST NURSE
If you had surgery for cancer you can contact your Specialist Nurse for advice.

Follow up
SURGEON
You will be sent an appointment to see your surgeon in a clinic. This is normally a few weeks after your operation
Research
NHS Lothian is committed to supporting clinical research. If you are eligible for any research studies, someone from the research team may contact you with information that you can read. If you do not wish to take part in any research, this will not affect your clinical care in any way.
PLEASE NOTE
This website includes content taken from the Royal College of Anaesthetists’ (RCoA) leaflets ‘Fitter, Better, Sooner (2018)’, ‘You and your anaesthetic (2020)’, ‘Anaesthesia explained (2015)’, and ‘Common events and risks in anaesthesia(2019)’. However, The RCoA has not reviewed the website as a whole. Some of the RCoA infographics used on the website have been adapted for web viewing.













