Inpatient Medicine for the Elderly and Stroke services for the north of Edinburgh are provided at the Western General Hospital. These pages provide information on our inpatient wards and the various liaison services we run to support the care of elderly patients across the hospital.
We aim to discharge patients home or a more homely environment as soon as possible with the correct support in place. Once the acute episode is completed patients may continue their rehabilitation in an interim or intermediate care unit at a different site, or supported by our Hospital at Home team.
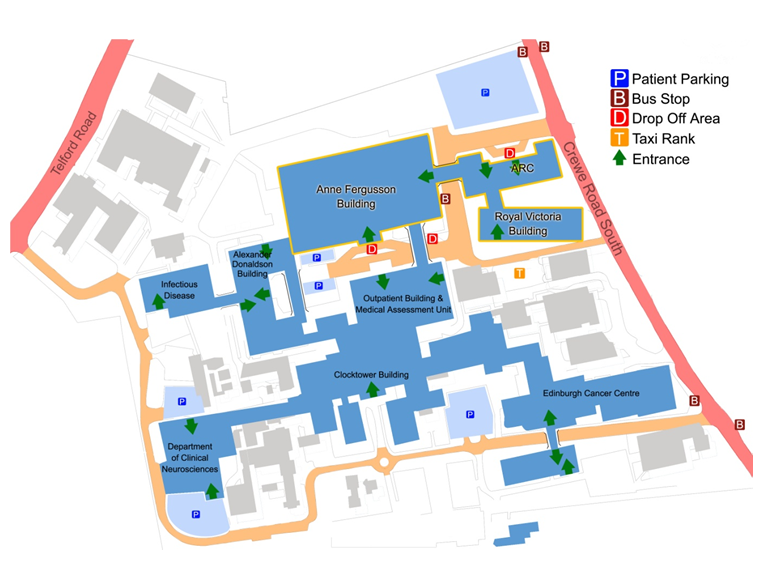
Our Medicine for the Elderly assessment and rehabilitation wards are located in the Anne Ferguson Building (Wards 50, 51 and 55) and the modern, purpose built Royal Victoria Building (wards 70, 71, 73, and 74). We work closely with social services from City of Edinburgh Council, West Lothian, Midlothian and East Lothian, and link with rest of NHS Lothian’s services across the city.
Elderly Medicine and Stroke Inpatients
We generally work to try and support elderly people to remain well at home. However, if someone does become unwell and they need to attend hospital and it is likely that they need to stay beyond 48 hours, we aim to admit them to one of our Assessment and Rehabilitation wards.
Most patients (young or old) who are admitted to the Western General having suffered a stroke should be moved to our Acute Stroke Unit within 24 hours. This is located in ward 71 in the Royal Victoria Building.
The Royal Victoria Building opened in 2012 to replace the older Royal Victoria Hospital on Craigleith Road. All the beds are located in single side rooms and the ward include day room areas. We encourage patients to spend time out of their rooms in the communal areas if at all possible. We also have our own patient gyms and assessment areas for physiotherapy and occupational therapy rehabilitation.
There is also an outdoor area to be enjoyed by patients and visitors that is easily accessible from the lower ground floor, as well as an Aroma coffee bar by the main entrance. PIC RVB garden As well as inpatient beds, we also run various day hospital and outpatient services. These are either based in the Royal Victoria Building’s Assessment and Rehabilitation Centre (ARC)
| Anne Fergusson Building | Role | Contact |
| Ward 50 | Elderly acute assessment and rehabilitation ward | 0131 537 3550 |
| Ward 51 | Elderly acute assessment and rehabilitation ward | 0131 537 3551 |
| Royal Victoria Building | ||
| Ward 70 | Elderly acute assessment and rehabilitation ward | 0131 465 9081 |
| Ward 71 | Acute stroke unit and stroke rehabilitation ward | 0131 465 9071 |
| Ward 72 | Medical admissions ward | 0131 465 9072 |
| Ward 73 | Orthogeriatric rehabilitation ward | 0131 465 9073 |
Visiting times
All of our Medicine for the Elderly and Stroke wards have opening visiting times from 10:00am to 8:00pm. Unless relatives are helping with meals however, we generally ask that visitors stay away during in protected mealtimes to help ensure patients are free to eat meals uninterrupted. NHS Lothian has more information on visiting hospital.
Rehabilitation and Discharge planning
Recovery in Hospital
When in hospital and recovering from an illness, our whole ward team helps to rehabilitate patients as much as possible. This includes our nursing staff, support works, and various therapists (e.g. physiotherapists, occupational therapists speech and language therapists), and dieticians, for example.
Each week, our wards hold a team meeting (MDT) where all staff comes together to plan the care for patients.
If you have any questions about the care of someone in hospital, please speak to ward staff. You can also meet with the ward medical staff or arrange to meet with their consultant if you have further questions.
Discharge Planning
Once patients are in hospital, the ward team, therapists and others work to try and get them better and back to how they were living before coming in to hospital, if possible. A large part of this can rely on community services, support from social work and carers and planning for discharge.
Each of our ward teams will have a team discussion about all the people on their ward to safely plan their discharge at the nearest opportunity. The ward staff would be able to provide updates on this progress, as appropriate.
Edinburgh council provides information on the different services that can help people live at home.
More information and emergency advice can be found through Social Care Direct.
Other Services
Liaison Services
Although we have dedicated ward for more elderly patients in the Western General Hospital, many older patients are looked after by other specialists. We support these patients in a variety of ways.
Our hospital liaison service is comprised of specialist doctors, nurses and therapists and service covers acute medicine, infectious diseases, colorectal surgery, urology, haematology and oncology. The team will screen older people for problems associated with frailty, and we support their treatment and recovery.
We often become involved as soon as possible for the day after a more frail person is admitted to the acute medical unit. Alternatively, we may be referred people who have been in hospital longer and require further rehabilitation.
Proactive Care of Older People in Surgery (POPS)
As well as supporting people in hospital already we also help plan the care of people who may need a surgical procedure in the future. This is often procedures done by the urology and colorectal teams in the hospital. People who are more elderly or would be thought to benefit from this may be seen by the team before their procedure to help decide if it is the right thing to do and how best to plan to do it safely.
Issues affecting people in hospital
When elderly and frail patients are admitted to hospital, they are not only more unwell to begin with, but also unfortunately but at risk of further problems. Although we prioritise both helping people recover from an illness as much as possible, and also doing everything we can to prevent further problems during their stay, we know that some problems can stiff occur.
Common problems include people falling, becoming more confused (delirious), pressure ulcers, or suffering further infections. Unfortunately, despite everyone’s best efforts more elderly and frail patients will always be at risk of these problems. Some more information about these can be found below.
| Falls | We shouldn’t accept falls as a normal part of getting older. It’s true that as we age our chances of having a fall increase, but falls are caused by a number of risk factors that can affect a person of any age. Unfortunately, being in hospital can put elderly people at risk of falling and all our staff work hard to recognise this risk and take measures to reduce falls and injuries wherever possible. NHS Inform Causes of Falls |
| Pressure Ulcers | Pressure ulcers are an injury that breaks down the skin and underlying tissue. They are caused when an area of skin is placed under pressure. They are sometimes known as “bedsores” or “pressure sores”. NHS Inform information on Pressure Ulcers |
| Delirium | Delirium is a common, serious but often treatable condition that starts suddenly in someone who is unwell. It’s much more common in older people, especially those with dementia. More information can be found on the Alzheimer’s Scotland website. |
| Getting to Know Me | Getting to know me is a document filled in by the person with dementia as much as possible, or by a family carer or relative, with the help of hospital staff if necessary. It is then held with the person’s notes so it is readily accessible to all staff working with that individual. Getting to know me aims to give hospital staff a better understanding of patients with dementia who are admitted either for planned treatment, such as an operation, or in an emergency. Information on Getting to Know Me Campaign |
| What Matters to you | As healthcare professionals, we want to promote careful, kind human interactions. Asking “What matters to you?” is about understanding what matters to an individual in their life. It’s about having meaningful conversations with individuals, as well as their families and carers. These conversations can help inform decisions about a person’s health and care. When we engage with individuals about their health and care decisions, it can greatly improve their wellbeing and outcomes. What Matters to You? |
| Adults with incapacity | When someone is unwell or delirious in hospital and unable why they are there, they may struggle to consent to everything being done to help them. This is done under the Adults with Incapacity Act to make sure that what is being done is in their best interests and properly discussed with those close to them. More information can be found on the Mental Welfare Commissions website – Adults with Incapacity Act (2000) |
| Power of Attorney | When someone is unwell or delirious in hospital and unable to give their own consent to treatment or tests, their Power of Attorney can do so on their behalf. Everyone to register one or more Powers of Attorney for themselves, but they have to do so while they can understand what it means. There are two types of Power of Attorney. A Continuing Power of Attorney is someone who can look after your property and finances. A Welfare Power of Attorney is someone who you trust to make decisions about your health and care, but only if you are unable to do this yourself. Links MWC Information Office of the Public Guardian Information Office of the Public Guardian – Top 10 Tips Age UK Information |
Standards of Care and Inspections
We are committed to providing high quality care and have a rigorous programme of clinical audit and quality improvement activity within the department. Like all health and social care services, our department and the Western General Hospital are regularly assessed by Health Improvement Scotland. The most recent reports many be accessed here.














